Mimi Burke of Crown Point says balancing Indiana’s Medicaid shortfall on the backs of the state’s most vulnerable residents will be devastating and cruel.
Burke’s daughter, Sophia Burns, 21, is considered medically complex. Burns has Rett syndrome and is confined to a wheelchair and uses a feeding tube for her nutritional needs. Burns requires 24-hour care, which Burke has provided since her daughter’s birth.
Since August, Burke has participated in the attendant care program which has helped ease the financial burden caring for a medically complex child has had on her family, which includes her second husband Mike Burke and her son Calen Burns. The family sacrifices daily to make Sophia’s life as comfortable and normal as possible inside their Crown Point home.
Crown Point resident Sophia Burns, who has Rett Syndrome, works with Crown Point Schools speech language pathologist Adrian Herrenbruck during a speech therapy session on Jan. 25, 2024. (
“We haven’t been on the program for long. Just based on how long we’ve been on the program, it has been life changing for us,” Burke said.
In December, a state budget outlook found that Indiana’s Medicaid budget would fall about $1 billion short over its current two-year funding cycle which includes 2024 and 2025. Among the proposed changes from the Indiana Family and Social Services Agency to shore up the Medicaid budget is eliminating the attendant care program.
On Thursday, the Republican supermajority in the House killed HB 1386, a “Medicaid Matters” bill, by failing to call it for second reading after 10 amendments were filed to clarify the Medicaid waivers under home- and community-based services in the wake of uproar from advocates and individuals across the state.
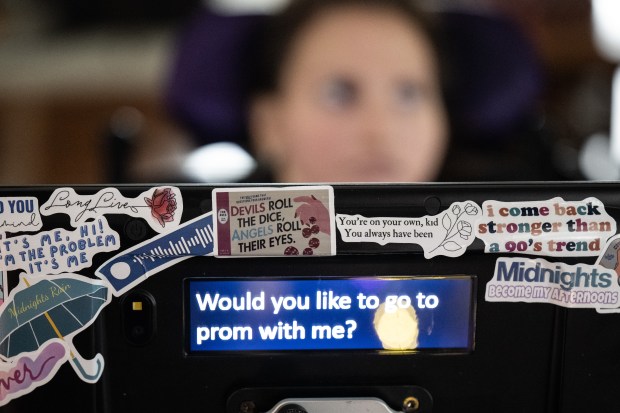
Crown Point resident Sophia Burns, who has Rett Syndrome, practices a prom proposal with her speech language pathologist, Adrian Herrenbruck, during a speech therapy session on Jan. 25, 2024.
Lt. Gov. Suzanne Crouch on Monday called FSSA to find another way to balance its budget instead of looking at the attendant care services.
The program was approved on the federal level in 2017 and funding was made available, but Indiana did not opt into the program until 2022 during the pandemic when the effects of a statewide nursing shortage became evident.
“The program was created well before the pandemic was on anybody’s radar,” Burke said. She called blaming the funding shortfall on a need created by the pandemic is disingenuous.

Mimi Burke, whose daughter, Sophia, suffers from Rett Syndrome, speaks about the impact that FSSA funding cuts will have on her family on Jan. 25, 2024.
Michelle Holtkamp, FSSA’s director of communications and public affairs, did not respond to repeated requests for comment, including how many families would be impacted by the proposed changes.
Lives of families like Burke’s could be upended depending on what changes go through in the final budget.
“If this program is cut the way they are proposing, it will be devastating for my family and thousands of families with medically complex children,” Burke said.

Crown Point resident Mimi Burke, on left, and her daughter Sophia, who has Rett Syndrome, work with Crown Point Schools speech language pathologist Adrian Herrenbruck during a speech therapy session on Jan. 25, 2024.
Under the current program, Burke can be a paid caregiver but cannot be paid for the time she provides medical-level care. So when it’s time to feed Sophia, Burke says she has to clock out. If the cuts go through, Burke said — as Sophia’s parent — she would no longer be paid for the hours she spends caring for Sophia. Instead, the family can find another relative or stepparent to take her place.
“They no longer want to pay parents or legal guardians, but an aunt or cousin or other extended family member can participate in the program. What they are saying is we will pay somebody else. We just don’t want to pay the parent,” Burke said.
The catch is, those individuals cannot provide the medical-level care such as feeding, so the parent has to be present whether an outside family member is providing care or not.
“They know that for most families, that random person doesn’t exist,” Burke said.
While the program provides needed financial assistance and some stability to Burke and families like hers across the state, she does not want anybody to think the money paid to parental caregivers lets them live a life of luxury.
“We’re not thriving on this program. We’re not going on extravagant vacations. We’re just kind of playing catch up and surviving,” Burke said.
“I can’t work,” Burke said. She worked as a nurse at Methodist Hospitals for 12 years, but was fired 12 years ago because it was too much for them to continue to work around her schedule. She said they tried and could sympathize but could not do it from a business perspective anymore.
“That’s the situation a lot of medically complex families face,” Burke said.
Some families have nursing, and Burke said at one time they did too. But qualified home health nurses are hard to find because their pay is significantly less in the home setting. Even when they had nursing care, it was only for a few days a week and not the 24 hours a day Sophia requires.
Each family must go through a process in order to qualify for the program, outlining in 15-minute increments how their time is spent. The state then determines the number of qualified hours a day the parent can be paid as a caregiver. The qualifying parent earns about $13 to $15 an hour instead of the daily rate to provide under the structured family care program. That rate is about $48.
The daily rate comes to about $1,300 a month, a figure well below the poverty level.
Teresa Torres with Everybody Counts said it is not surprising Indiana wants to balance its Medicaid budget on the backs of the state’s most vulnerable residents. Funding for programs benefiting people with disabilities is often the first to be cut to fill budget gaps.
Loss of the program will mean some clients no longer will be able to keep their loved ones in their homes, ultimately having to transfer them to a group home, assisted living, or nursing facility. Torres said the long-term care these individuals need when they can no longer be cared for in their homes costs more than the hourly pay family caregivers receive to keep that person out of a facility.
Torres said the attacks on services for those with disabilities create a sense of otherness.
“This helps create the illusion, create the impression, among the general public ‘those people’ cost us money,” she said.
“It’s not that it is not working…It’s just an easy target,” Torres said. A lack of accounting for the number of families utilizing the program, its costs and its success or failure has not been forthcoming from state officials.
Torres said the program allows those families to be able to stay together with minimal impact on the family as opposed to those families having no choice but to tear themselves apart. It also ultimately represents a cost savings by keeping individuals out of long-term care facilities, she said.
“What this action is, is a reflection on Indiana’s lack of respect and concern for individuals with disabilities and their family members,” Torres said. The system has been created to dehumanize people and tear them from their families while spending a fortune on brand new facilities to house people, she said.
“(The rules change) is ripping families apart,” Torres said.
The people using home health care cannot even be authorized for the amount of care they actually need. A nursing shortage means people will struggle to find caregivers for even the reduced hours of care they need. Care often falls back to parents and family, who then have to choose between work and providing full-time care. Without compensation, the need to care for their family members can have devastating financial consequences.
“What this is going to do to families is unconscionable. It’s absolutely unconscionable,” Torres said.
For Susan Naden, mother to Braxson Jones, 6, the rules change means her husband is unable to adopt Braxson and his older brother.
Plans underway for the adoption this spring now are on hold. Braxson is a medically complex child after he was a victim of shaken baby syndrome at 6 months old at the hands of this father, Curtis Jones. Jones was sentenced to 10 years in prison for the crime.
Braxson is now blind, receives his nutrients from a feeding tube and needs 24-hour care. Naden said she remarried four years ago and she was able to adopt her new husband’s daughter. The boys have anxiously awaited their turn at adoption. It took years for their birth father to sign off, she said.
“It’s not going to affect us financially,” Naden said, adding her husband will be able to be paid to care for Braxson. Their family, however, will not be able to share the same name. Now, under the FSSA rules change, only stepparents can provide attendant care, meaning the boys will not be able to be adopted.
“It’s kind of stupid,” Naden said as assistance for parents with children of disabilities already is limited.
As a single mom earning $30,000 a year, she did not qualify for Medicaid, SNAP or disability for her son because her earnings were too high.
Naden worked as a nurse until May 2022 when she qualified for the program. She now works as a nurse in her home caring for her son.
“He’s always been with us,” she said.
Fortunately, the family will be able to weather the change financially, she said.
“Some of these people are probably single parents. It’s going to impact them,” she said.
Leslie Hawker, board president for Everybody Counts, and Jordan Musenbrock, a counselor advocate, said as word gets around about the proposed cuts, calls from concerned clients will begin to grow. They said clients depend on the money, often to pay their bills or help cover transportation and care costs for their family member.
“It definitely will impact all of the centers,” Musenbrock said. “I think we are going to be getting a lot of calls from angry, upset, lost parents looking for help.”
Part of their role is being prepared to have something to tell these families when they call, to advocate with them and to fight back.
“We’re not OK with this,” Musenbrock said. “This is a big deal. This is income for a lot of families, this is like a car payment to some people, or a house payment. The impact that it will have on families in the state I can’t put into words. The negative outcome. There’s no words. It’s just sad.”




